Abstract
The role of glutamatergic dysfunction in the pathophysiology of OCD has hardly been explored despite recent reports implicating glutamatergic dysfunction in OCD. We decided to investigate CSF glutamate levels in adult OCD probands compared to psychiatrically normal controls. In total, 21 consenting psychotropic drug-naïve adult OCD patients, diagnosed using SCID-IV-CV, and 18 consenting psychiatrically normal controls with age within 10 years of age of the patients, who did not have any history of head injury or neurological illness, were included into the study. Aseptically collected and stored CSF samples obtained from the patients and control subjects were used for glutamate estimation, which was carried out by a modification of the procedure described by Lund (1986). CSF glutamate (μmol/l) level was found to be significantly higher [F(1,31)=6.846, p=0.014] in OCD patients (47.12±4.25) compared to control subjects (41.36±3.63) on analysis of covariance. There was no effect of gender, age, duration of illness, Y-BOCS score, or CGI-S score on CSF glutamate levels. Our study provides preliminary evidence implicating glutamatergic excess in the pathophysiology of OCD, which needs to be further explored by studies from other centers involving larger sample sets from different age groups.
Similar content being viewed by others
INTRODUCTION
There is now a large body of evidence regarding the serotonergic basis of OCD. Functional imaging studies have also implicated cortico-striatal-pallido-thalamo-cortical tract dysfunction in OCD patients (Saxena et al, 1998). These regions also receive a large amount of serotonergic innervation from the raphe nuclei. While the exact nature of serotonergic dysfunction in OCD is still a matter of conjecture, the fact that at least 30% of OCD patients do not respond to specific serotonin reuptake inhibitors (SSRIs) indicate that there might be different mechanisms underlying the overall clinical heterogeneity of OCD patients (Montgomery, 1994; Sasson and Zohar, 1996). The fact that only approximately 50–60% of OCD patients report exacerbation of symptoms after acute administration of m-CPP serves as a further pointer to the role of other neurotransmitters in OCD. While some meta-analyses (Griest et al, 1995; Stein et al, 1995) suggest that less selective serotonergic agents may be more efficacious in OCD, the fact that OCD patients with comorbid tics respond better on augmentation of SSRIs with antipsychotics also support the role of other factors in OCD. Although, researchers have investigated the role of the opioid system (Keuler et al, 1996) and neuropeptides like oxytocin and vasopressin (Altemus et al, 1992; Leckman et al, 1994) in OCD, the evidence has been equivocal.
One of the neurotransmitters that have not been investigated till recently with relation to OCD, despite being present in abundance in the neuroanatomical substrate implicated in OCD, has been glutamate. Although functional, structural, and spectroscopic brain imaging studies have implicated dysfunction in either the ‘direct’ or ‘indirect’ loops of the cortico-striato-pallido-thalamo-cortical OCD circuit (Saxena and Rauch, 2000), where the predominant excitatory neurotransmitter is glutamate, there have been few hypothesis-driven studies investigating glutamatergic dysfunction in OCD. In one of the first reports implicating glutamatergic dysfunction in OCD, Moore et al (1998) reported striking changes in caudate glutamate resonance on proton magnetic resonance spectroscopy (1H-MRS) in a 9-year-old boy with OCD following 12 weeks of paroxetine treatment. Subsequently, Rosenberg et al (2000) studied 11 psychotropic drug-naïve children (8–17 years) with OCD, with single-voxel 1H-MRS examinations and demonstrated that caudate glutamate concentrations were significantly greater in the patients compared to healthy controls. They also found that the caudate glutamate levels in patients decreased significantly following 12-weeks treatment with paroxetine to levels comparable to that of controls and the decrease was associated with decrease in symptom severity of the OCD patients. In the same study, they also compared the glutamate levels in occipital cortex in another sample of eight pediatric OCD patients and eight healthy children and found no difference between the two. In a subsequent report (Bolton et al, 2001), the same group reported that the decrease in left caudate glutamate levels on 1H-MRS following 12 weeks treatment with paroxetine, persisted 3 months after medication discontinuation in an 8-year old girl, who was part of the earlier sample of paroxetine treated OCD patients. The authors however did not find any significant change in left caudate volumes between baseline, after 12 weeks of paroxetine and 3 months after discontinuation of paroxetine.
Although, the 1H-MRS studies implicate glutamatergic dysfunction in OCD, the studies involved small samples and only pediatric age group. To our knowledge, there are no published reports that have investigated glutamatergic dysfunction in adult OCD. Although, studies have investigated glutamate levels in CSF in schizophrenia (Kim et al, 1980; Gattaz et al, 1982; Korpi et al, 1987; Labarca et al, 1995; Faustman et al, 1999), similar studies are lacking in OCD. In the background of the MRS data, we decided to investigate CSF glutamate levels in adult OCD probands and compare it to psychiatrically normal controls.
MATERIALS AND METHODS
Recruitment and Assessment of Subjects
The study was approved by the departmental review board and was in accordance with the Helsinki declaration, 1975. All patients aged 16 years and older, screened at the National Institute of Mental Health and Neurosciences (NIMHANS) Psychiatry Screening OPD and diagnosed to be suffering from OCD, and who had never been on any psychotropic agents were administered the Structured Clinical Interview for DSM IV-clinician version (SCID-IV-CV) (First et al, 1997). Patients who fulfilled the diagnostic criteria, and who did not have any lifetime history of psychotic disorder or mental retardation, were included in the study. Informed consent of patients was taken before including them in the study. Thereafter, patients were rated on the Yale-Brown Obsessive Compulsive Symptom Checklist (Y-BOCS) (Goodman et al, 1989a, 1989b), Yale-Brown Obsessive Compulsive Severity Rating Scale (Goodman et al, 1989a, 1989b), and Clinical Global Impression- Severity (CGI-S) Scale. In total, 21 consenting psychotropic drug-naïve OCD patients were included into the study. Control population were taken from patients scheduled for various operative procedures (n=12; inguinal hernia—5, fractures of the femur and tibia—4, varicocele—1, anal fissure—1 and fibroid uterus—1) under spinal anesthesia in a general hospital located in the same geographical area and also from staff (n=6) working in the hospital who volunteered to be part of the study. Informed consent was taken before finally including the subjects into the study. They were included into the study following administration of SCID-IV-CV (First et al, 1997) after ruling out lifetime history of any psychiatric illness and history of head injury or any other neurological illness. In total, 18 consenting psychiatrically normal controls without any history of head injury or other neurological illness and with age within 10 years of age of the patients were taken into the study. Subsequently, lumbar puncture was carried out to collect CSF.
Sample Collection and Storage
Lumbar puncture was carried out in patients as well as controls after overnight fasting. About 2 ml of CSF was collected, under aseptic conditions from the intervertebral space between L4 and L5 spines, using 22 gz disposable spinal needles with the subject in the left lateral position. The CSF sample was transferred in ice-packs and immediately stored at −70°C. We did not employ any dietary restrictions for either the patients or controls in this study. The stored CSF was used subsequently for glutamate estimation. The duration of storage before estimation of the CSF sample was between 2 and 20 months (mean=12.95±5.15) for the patient sample and 2 and 11 months (mean=3.02±2.90) for the control sample.
Glutamate Estimation
Glutamate estimation was carried out by a modification of the procedure described by Lund (1986). Briefly, various concentrations of Glutamate standards obtained from Sigma-Aldrich (USA) were taken in screw-capped tubes marked ‘S’ while 0.25 ml of patient samples were taken in screw-capped tubes marked ‘T’. To each of the standard or test samples, 1 ml of Tris-EDTA-Hydrazine buffer, 0.1 ml of NAD solution, 0.01 ml of ADP solution, and water were added, so that the total reaction volume added up to 2 ml (Tris-EDTA-Hydrazine buffer, NAD, and ADP solution obtained from Sigma-Aldrich, USA). Absorbance (C1) was read using a spectrophotometer at 340 nm to obtain background reading. To each of the tubes, 0.02 ml of L-glutamic dehydrogenase was added and the absorbance (C2) was again read after a 40-min incubation, at 340 nm subtraction of C1 from C2 gave the net absorbance. The calculation of the glutamate level in the samples was carried out using the standard curve.
Statistical Analysis
Initially, we analyzed differences in sociodemographic variables between the two groups (OCD vs normal controls) with χ2 test for categorical variables and Student's t-test for continuous variables. Means and frequencies of clinical variables in the OCD group were calculated. We examined a scatter-plot of CSF glutamate levels to identify outliers. To investigate whether CSF glutamate levels differed between the two groups of subjects, we did analysis of covariance (ANCOVA) using diagnosis and gender as factors and age, duration of illness, Y-BOCS scores, and CGI-S scores as covariates and repeated this analysis after excluding the outliers.
RESULTS
Demographic and Clinical Characteristics
Table 1 shows the sociodemographic profile of the subjects. There were no significant differences between the OCD patients and the controls except that the mean age of the control group was significantly more compared to the patient group. Table 2 shows the mean duration of illness, mean Y-BOCS and CGI- S scores, psychiatric comorbidities and frequencies of various obsessive- compulsive symptoms in the patients.
CSF Glutamate levels
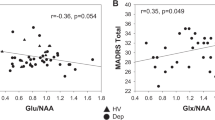
Table 3 shows the mean glutamate levels (μmol/l) in CSF in male and female patients and controls. Figure 1 shows a scatter-plot of CSF glutamate levels in male and female patients and controls. Table 4 shows the result of analysis of covariance (ANCOVA) with diagnosis and gender included as factors and age, duration of illness, total Y-BOCS scores, and CGI-S scores included as covariates. There was a significant main effect (p=0.014) of diagnosis on CSF glutamate levels. No statistically significant effect of gender, age, duration of illness, total Y-BOCS scores, or CGI-S scores was found on differences in CSF glutamate levels between patients and controls. On repeating the ANCOVA after excluding the two outliers (one each from the patient and control group, as evident from the scatter-plot in Figure 1), we found that CSF glutamate levels were significantly higher in OCD patients compared to controls [F(1,29)=11.153, p=0.002]. Again, there was no statistically significant effect of gender, age, duration of illness, total Y-BOCS scores, or CGI-S scores on differences in CSF glutamate levels on repeating ANCOVA without the outliers.
DISCUSSION
The aim of our study was to investigate glutamate levels in psychotropic drug-naive OCD patients and compare it with psychiatrically normal controls. The main finding of our study is that CSF glutamate levels are significantly raised in OCD patients compared to normal controls, and that the difference is unrelated to age or gender of the subjects.
To our knowledge, this is the first published report investigating CSF glutamate levels in OCD patients, although there have been previous studies investigating various biogenic amines in CSF in OCD patients (Thoren et al, 1980; Insel et al, 1985; Swedo et al, 1992; Leckman et al, 1995). The use of psychotropic drug-naïve patients in order to avoid the confounding effects of medications (Charney et al, 1981; Mellstrom et al, 1982; Garvey et al, 1984) and the use of a psychiatrically normal control sample constitute the other methodological advantages of our study. While previous imaging studies have demonstrated increased glutamate levels, which come down with treatment, they had used pediatric sample. Our study demonstrates glutamatergic abnormalities for the first time in a sample of adult OCD patients. Additionally, one of the pitfalls of using 1H-MRS for estimating glutamate/glutamine levels is that they do not appear as a single resonance peak in the spectrum as N-acetyl aspartate (NAA) or choline (Cho) do, but are split into multiplets due to their chemical structures. In addition to limitations in absolute spectroscopic quantification, there is a large amount of overlap in the chemical shift range of the multiplets obtained from glutamate/glutamine, rendering such assessments imprecise. Thus, our study complements MRS imaging studies in providing an estimate of brain glutamate levels.
However, the results of our study need to be considered on the background of certain methodological limitations. Although the CSF samples in our patient and control sample were drawn following an overnight fast, the time of collection of the samples was not uniform for the patient and control samples. However, to our knowledge, there are no reports indicating diurnal variation in CSF glutamate levels.
We did not control for diet or collect data regarding body weight or basal metabolic index (BMI) of the subjects. Again there are no reports indicating dietary influence on CSF glutamate levels. A recent study also did not find any effect of weight, height, or BMI on CSF glutamate levels (Altemus et al, 2004). Our control sample was also not sex-matched with the patient sample and although attempt was made at matching age, the mean age of the control sample was significantly higher than the patient sample. However, previous studies that have looked at this issue have reported no influence of age and gender on CSF glutamate levels (Gjessing et al, 1974; Lakke and Teelken, 1976; McGale et al, 1977; Goodnick et al, 1980; Hagenfeldt et al, 1984; Ferraro and Hare, 1985, Altemus et al, 2004). In addition, our covariate analyses did not show any significant effect of age or gender on CSF glutamate levels. Studies have, however, found that CSF glutamate levels varied according to mode of collection and storage (Ferrarese et al, 1993). Levels of untreated CSF glutamate have been found to decrease gradually over time (Ferrarese et al, 1993; Anesi et al, 1998). Although we used untreated CSF for glutamate estimation, as our patient's samples were stored for a longer duration compared to our control samples, the significantly higher glutamate levels found in our patient samples are unlikely to be an artifact of storage condition. On the contrary, possibly the differences would have been higher if our CSF samples were treated with acid and neutralized, or analyzed faster after collection. Some of our control subjects were scheduled for operative procedures for various conditions. It is unlikely that the CSF glutamate levels were influenced by these procedures as the CSF samples were obtained before the subjects were anesthetized for these procedures. To our knowledge, there is also no evidence that any of the various physical conditions present in our control subjects have any effect on CSF glutamate levels. It is also possible that CSF glutamate levels change with the stress of lumbar puncture as previously reported for various other neurochemicals, and thus do not reflect the correct levels (Hill et al, 1999). However, this would have equally affected both the patient and control groups and hence would be unlikely to result in different CSF glutamate levels in the two groups.
Our study shows no statistically significant effect of total Y-BOCS scores or CGI-S scores on CSF glutamate levels, when they were included as covariates in the ANCOVA. If CSF glutamate levels were to be causally linked to OCD, one would expect an effect of symptom severity as measured by Y-BOCS or CGI-S scores on CSF glutamate levels, which was not found in our analyses. There are various possible explanations for this finding. It is possible that our study sample was underpowered to delineate the relationship between OCD symptom severity and CSF glutamate levels. A more likely reason for the lack of statistically significant relationship between OCD symptom severity and CSF glutamate levels as evident in our study is that although our study and various neuroimaging studies implicate glutamatergic excess in the pathophysiology of OCD, it is likely that there is a complex interplay of various neurotransmitter dysfunctions rather than centrality of one neurotransmitter dysfunction in OCD, ruling out any simple correlation between OCD symptom severity scores and CSF glutamate levels. It is also possible that there are hyposerotonergic and hyperglutamatergic subtypes of OCD and any relationship between measures of symptom severity and CSF neurotransmitter levels are likely to be manifest only when patients with a specific neurotransmitter dysfunction are selected in a study.
The results of our study implicate glutamatergic excess in the pathophysiology of OCD. This needs to be understood on the background of the current understanding regarding the neurobiological basis of OCD. On the basis of functional, structural, and spectroscopic brain imaging studies, it has been postulated that OCD involves dysfunction in one of the several hypothesized parallel cortico-striato-pallido-thalamo-cortical loops (Alexander et al, 1986; Saxena and Rauch, 2000). The OCD circuit is hypothesized to have two loops: (1) the direct pathway, projecting from the cerebral cortex to striatum to the internal segment of the globus pallidus-substantia nigra-pars reticulata complex (Gpi/SNr) and then to thalamus and back to cortex; and (2) the indirect pathway, projecting from the cortex to striatum and then to the external segment of the globus pallidus followed by subthalamic nucleus before returning to the Gpi/SNr, where it rejoins the common pathway to the thalamus before returning to the cortex (Saxena and Rauch, 2000). Although there are various neurotransmitters that modulate the activity of afferents and efferents in these loops, it is significant that excitatory inputs in these pathways are predominantly glutamatergic, whereas inhibitory ones are predominantly GABAergic (Parent and Hazrati, 1995). It has been hypothesized that overactivity of the direct pathway or underactivity of the indirect pathway leads to OCD. Considering the predominant neurotransmitters involved in these pathways, the direct pathway overactivity model of OCD suggests glutamatergic excess in certain brain regions in OCD, which is compatible with increased CSF glutamate in OCD patients. Thus, our finding of significantly increased CSF glutamate in OCD patients provides evidence in support of the current neurobiological models of OCD. However, one needs to keep in mind that increased CSF glutamate is not exactly the same as increased glutamatergic activity in the cortical and subcortical pathways. Different processes such as neuronal release and transport, glial uptake, diffusion barriers, sequestration in distinct metabolic pools, and degradation may be responsible for the modifications of glutamate levels in CSF. Nevertheless, various studies have demonstrated the existence of a blood–CSF barrier to amino acids and suggested that CSF glutamate concentrations should reflect its function within the central nervous system (McGale et al, 1977; Ijima et al, 1978; Kornhuber and Kornhuber, 1992; Rothstein et al, 1992).
The findings of our study that glutamatergic dysfunction is related to the pathophysiology of OCD has been supported also by findings from animal studies, in addition to the MRS-imaging studies in pediatric OCD (Moore et al, 1998; Rosenberg et al, 2000; Bolton et al, 2001). McGrath et al (2000) have shown that MK-801, a noncompetitive NMDA receptor antagonist that indirectly stimulates cortical-limbic glutamate output, aggravated a transgene-dependent abnormal behavior (repetitive climbing and leaping) in a transgenic mouse model of comorbid Tourette's syndrome and OCD, at doses insufficient to induce stereotypies, and more readily induced stereotypies and limbic seizure behaviours at higher doses.
In summary, our study provides preliminary evidence implicating glutamatergic excess in the pathophysiology of OCD. However, these findings need to be further explored by studies from other centers involving larger sample sets from different age groups. There is also a need to investigate the effect of treatment on CSF glutamate levels alongwith further characterization of various glutamate receptor levels and functioning in OCD patients before one may conclude on its relevance to OCD.
References
Alexander GE, DeLong MR, Strick PL (1986). Parallel organization of functionally segregated circuits linking basal ganglia and cortex. Annu Rev Neurosci 9: 357–381.
Altemus M, Fong J, Yang R, Damast S, Luine V, Ferguson D (2004). Changes in cerebrospinal fluid neurochemistry during pregnancy. Biol Psychiatry 56: 386–392.
Altemus M, Pigott T, Kalogeras KT, Demitrack M, Dubbert B (1992). Abnormalities in the regulation of vasopressin and corticotropin releasing factor secretion in obsessive-compulsive disorder. Arch Gen Psychiatry 49: 9–20.
Anesi A, Rondanelli M, d'Eril GM (1998). Stability of neuroactive amino acids in cerebrospinal fluid under various conditions of processing and storage. Clin Chem 44: 2359–2360.
Bolton J, Moore GJ, MacMillan S, Stewart CM, Rosenberg DR (2001). Case study: caudate glutamatergic changes with paroxetine persist after medication discontinuation in pediatric OCD. J Am Acad Child Adolesc Psychiatry 40: 903–906.
Charney DS, Heninger GR, Sternberg DE, Redmond DE, Leckman JF, Maas JW, Roth RH (1981). Presynaptic adrenergic receptor sensitivity in depression. The effect of long-term desipramine treatment. Arch Gen Psychiatry 38: 1334–1340.
Faustman WO, Bardgett M, Faull KF, Pfefferbaum A, Csernansky JG (1999). Cerebrospinal fluid glutamate inversely correlates with positive symptom severity in unmedicated male schizophrenic/schizoaffective patients. Biol Psychiatry 45: 68–75.
Ferrarese C, Pecora N, Frigo M, Appollonio I, Frattola L (1993). Assessment of reliability and biological significance of glutamate levels in cerebrospinal fluid. Ann Neurol 33: 316–319.
Ferraro TN, Hare TA (1985). Free and conjugated amino acids in human CSF: influence of age and sex. Brain Res 338: 53–60.
First MB, Spitzer RL, Gibbon M, Williams JBW (1997). Structured Clinical Interview for DSM-IV Axis I Disorders-Clinician Version (SCID-CV). American Psychiatric Press: Washington, DC.
Garvey MJ, Tuason VB, Johnson RA, Valentine RH, Cooper TB (1984). Elevated plasma tricyclic levels with therapeutic doses of imipramine. Am J Psychiatry 141: 853–856.
Gattaz WF, Gattaz D, Beckmann H (1982). Glutamate in schizophrenics and healthy controls. Arch Psychiatr Nervenkr 231: 221–225.
Gjessing LR, Gjesdahl P, Dietrichson P, Presthus J (1974). Free amino acids in the cerebrospinal fluid in old age and in Parkinson's disease. Eur Neurol 12: 33–37.
Goodman WK, Price LH, Rasmussen SA, Mazure C et al (1989a). The Yale-Brown obsessive-compulsive scale: I. Development, use and reliability. Arch Gen Psychiatry 46: 1006–1011.
Goodman WK, Price LH, Rasmussen SA, Mazure C et al (1989b). The Yale-Brown obsessive-compulsive scale: II. Validity. Arch Gen Psychiatry 46: 1012–1016.
Goodnick PJ, Evans HE, Dunner DL, Fieve RR (1980). Amino acid concentrations in cerebrospinal fluid: effects of aging, depression, and probenecid. Biol Psychiatry 15: 557–563.
Griest JH, Jefferson JW, Kobak KA, Katzelnick DJ, Serlin RC (1995). Efficacy and tolerability of serotonin transport inhibitors in obsessive-compulsive disorder. A meta-analysis. Arch Gen Psychiatry 52: 53–60.
Hagenfeldt L, Bjerkenstedt L, Edman G, Sedvall G, Weisel FA (1984). Amino acid in plasma and CSF and monoamine metabolites in CSF: interrelationship in healthy subjects. J Neurochem 42: 833–837.
Hill KK, West SA, Ekhator NN, Bruce AB, Wortman MD, Bake DG et al (1999). The effect of lumbar puncture stress on dopamine and serotonin metabolites in human cerebrospinal fluid. Neurosci Lett 276: 25–28.
Ijima K, Takase S, Tsumuraya K et al (1978). Changes in free amino acids of cerebrospinal fluid and plasma in various neurological diseases. Tohuku J Exp Med 126: 133–150.
Insel TR, Mueller EA, Alterman I, Linnoila M, Murphy DL (1985). Obsessive-compulsive disorder and serotonin: is there a connection? Biol Psychiatry 20: 1174–1188.
Keuler DJ, Altemus M, Michelson D, Greenberg B, Murphy DL (1996). Behavioral effects of naloxone infusion in obsessive-compulsive disorder. Biol Psychiatry 40: 154–156.
Kim JS, Kornhuber HH, Schmid-Burgk W, Holzmuller B (1980). Low cerebrospinal fluid glutamate in schizophrenic patients and a new hypothesis on schizophrenia. Neurosci Lett 20: 379–382.
Kornhuber ME, Kornhuber J (1992). Cerebrospinal fluid amino acids in amyotrophic lateral sclerosis. Ann Neurol 31: 449–450.
Korpi ER, Kaufmann CA, Marnela KM, Weinberger DR (1987). Cerebrospinal fluid amino acid concentrations in chronic schizophrenia. Psychiatry Res 20: 337–345.
Labarca R, Silva H, Jerez S, Ruiz A, Renterias P, Ogalde C et al (1995). Effects of haloperidol on CSF glutamate levels in drug-naive schizophrenic patients. Schizophr Res 16: 83–85.
Lakke JP, Teelken AW (1976). Amino acid abnormalities in cerebrospinal fluid of patients with parkinsonism and extrapyramidal disorders. Neurology 26: 489–493.
Leckman JF, Goodman WK, Anderson GM, Riddle MA, Chappell PB, McSwiggan-Hardin MT et al (1995). Cerebrospinal fluid biogenic amines in obsessive compulsive disorder, Tourette's syndrome, and healthy controls. Neuropsychopharmacology 12: 73–86.
Leckman JF, Goodman WK, North WG, Chappell PB, Price LH, Pauls DL et al (1994). The role of central oxytocin in obsessive compulsive disorder and related normal behavior. Psychoneuroendocrinology 19: 723–749.
Lund P (1986). L-Glutamine and L-Glutamate: UV method with Glutaminase and Glutamate Dehydrogenase. In: Bergmeyer HU (ed). Methods in Enzymatic Analysis, Vol 8. VCH, Verlagsgesellschaft: Weinhein. pp 357–363.
McGale EH, Pye IF, Stonier C, Hutchinson EC, Aber GM (1977). Studies of the inter-relationship between cerebrospinal fluid and plasma amino acid concentrations in normal individuals. J Neurochem 29: 291–297.
McGrath MJ, Campbell KM, Parks III CR, Burton FH (2000). Glutamatergic drugs exacerbate symptomatic behaviour in transgenic model of comorbid Tourette's syndrome and obsessive-compulsive disorder. Brain Res 877: 23–30.
Mellstrom B, Alvan G, Bertilsson L, Potter WZ, Sawe J, Sjoqvist F (1982). Nortriptyline formation after single oral and intramuscular doses of Amitryptyline. Clin Pharmacol Ther 32: 664–667.
Montgomery SA (1994). Pharmacological treatment of obsessive-compulsive disorder. In: Hollander E, Zohar J, Marazziti D, Olivier B (eds). Current Insights in Obsessive-Compulsive Disorder. Wiley: Chichester. pp 215–226.
Moore GJ, MacMaster FP, Stewart C, Rosenberg DR (1998). Case study: caudate glutamatergic changes with paroxetine therapy for pediatric obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 37: 663–667.
Parent A, Hazrati LN (1995). Functional anatomy of the basal ganglia. I. The cortico-basal ganglia-thalamo cortical loop. Brain Res Brain Res Rev 20: 91–127.
Rosenberg DR, MacMaster FP, Keshavan MS, Fitzgerald KD, Stewart CM, Moore GJ (2000). Decrease in caudate glutamatergic concentrations in pediatric obsessive-compulsive disorder patients taking paroxetine. J Am Acad Child Adolesc Psychiatry 39: 1096–1103.
Rothstein JD, Martin LJ, Kuncl RW (1992). Decreased glutamate transport by the brain and spinal cord in amyotrophic lateral sclerosis. N Engl J Med 326: 1464–1468.
Sasson Y, Zohar J (1996). New developments in obsessive-compulsive disorder research: implications for clinical management. Int Clin Psychopharmacol Suppl 5: 3–12.
Saxena S, Brody AL, Schwartz JM, Baxter LR (1998). Neuroimaging and frontal-subcortical circuitry in obsessive-compulsive disorder. Br J Psychiatry 173 (suppl 35): 26–37.
Saxena S, Rauch SL (2000). Functional neuroimaging and the neuroanatomy of obsessive-compulsive disorder. Psychiatr Clin N Am 23: 563–586.
Stein DJ, Spadaccini E, Hollander E (1995). Meta-analysis of pharmacotherapy trials for obsessive-compulsive disorder. Int Clin Psychopharmacol 10: 11–18.
Swedo SE, Leonard HL, Kruesi MJ, Rettew DC, Listwak SJ, Berrettini W et al (1992). Cerebrospinal fluid neurochemistry in children and adolescents with obsessive-compulsive disorder. Arch Gen Psychiatry 49: 29–36.
Thoren P, Asberg M, Bertilsson L, Mellstrom B, Sjovist F, Traskman L (1980). Clomipramine treatment of obsessive-compulsive disorder. II. Biochemical aspects. Arch Gen Psychiatry 37: 1289–1294.
Author information
Authors and Affiliations
Corresponding author
Additional information
Work done at Biological Psychiatry Lab, Nimhans, Bangalore, India.
Rights and permissions
About this article
Cite this article
Chakrabarty, K., Bhattacharyya, S., Christopher, R. et al. Glutamatergic Dysfunction in OCD. Neuropsychopharmacol 30, 1735–1740 (2005). https://doi.org/10.1038/sj.npp.1300733
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300733
Keywords
This article is cited by
-
Polygenetic risk scores and phenotypic constellations of obsessive–compulsive disorder in clozapine-treated schizophrenia
European Archives of Psychiatry and Clinical Neuroscience (2024)
-
Blood glutamate scavenging as a novel glutamate-based therapeutic approach for post-traumatic brain injury anxiety and social impairment
Translational Psychiatry (2023)
-
Cortical glutamate and GABA are related to compulsive behaviour in individuals with obsessive compulsive disorder and healthy controls
Nature Communications (2023)
-
Glucose metabolism and AD: evidence for a potential diabetes type 3
Alzheimer's Research & Therapy (2022)
-
Possible actions of cannabidiol in obsessive-compulsive disorder by targeting the WNT/β-catenin pathway
Molecular Psychiatry (2022)